Melika Azim Zadegan: Patient Empowerment: Does it truly matter?
In our previous blog post, my colleague Catherine and I delved into a review of existing technologies for remote monitoring, exploring smart devices, robotics, and intelligent information and communication systems. Now, in this blog post, I aim to provide an exploration of the concept of Patient Empowerment—what it entails and why it holds such immense significance. Embracing the era of digital transformation in healthcare, patient empowerment emerges not merely as a philosophical ideal but as a tangible and achievable goal—a key to a healthier and more collaborative future in healthcare.
What is Patient Empowerment?
According to WHO, patient empowerment in healthcare refers to the process of assisting individuals in gaining control over their health, encouraging them to take initiative, solve problems, and actively participate in their care.
Four components have been reported as being fundamental to the process of patient empowerment. Firstly, understanding by the patient of his/her role is crucial. Additionally, the acquisition by patients of sufficient knowledge to be able to engage with their healthcare provider is essential. Moreover, patient skills and the presence of a facilitating environment play key roles in this process. Based on these four components, empowerment can be defined as:
“A process in which patients understand their role, are given the knowledge and skills by their health-care provider to perform a task in an environment that recognizes community and cultural differences and encourages patient participation 1.”
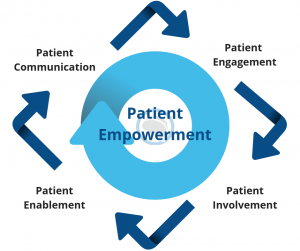
Figure 1: Voxello – “This is Now an Attainable Formula: Empowered Patient, Enhanced Communication, Better Outcomes”, Accessed: 12.04.2023
Patient empowerment should be seen as both an individual and a community process. This is achieved through the provision of relevant, appropriate, and user-friendly information by healthcare professionals, as well as through improved public health education initiatives.
Furthermore, patient empowerment leads to promoting self-health management, where individuals seek out information about their own illness. Additionally, it motivates patients to actively participate in treatment decisions, becoming a core value that encourages adherence to prescribed chronic therapies and involvement in self-management and preventative healthcare. The concept of patient empowerment has been extended to patient safety, employing strategies such as educational tools, motivation, reminder tools, and role modeling to empower patients.
Does Patient Empowerment Matter?
With the rise of digital health tools and the transition into the era of digitization and remote patient monitoring, the simple answer is YES!
Stepping into this digital landscape takes patient empowerment to new heights. Technological advancements offer patients unparalleled access to real-time health data, enabling continuous self-monitoring. Remote patient monitoring not only cultivates self-awareness but also streamlines communication with healthcare providers. The synergy between patient empowerment and digital health tools amplifies the potential for personalized, patient-centric care.
In essence, patient empowerment is the linchpin of a healthcare system aspiring to be genuinely patient-centered. It recognizes the pivotal role of individual agency, understanding that well-informed and engaged patients are more likely to adhere to prescribed therapies, actively participate in preventive healthcare, and ultimately achieve improved health outcomes.
How Can We Empower Patients?
Empowering patients involves a multifaceted approach, recognizing that a comprehensive strategy is essential for fostering active participation in healthcare decisions. Let’s delve into some of those:
1. Access to Information:
Providing patients with relevant, understandable information about their health conditions and treatment options is foundational to empowerment. This includes transparently sharing diagnoses, treatment plans, and potential outcomes. Beyond traditional channels, digital platforms can play a pivotal role in delivering accessible and personalized health information, enabling patients to make informed decisions about their well-being. Accessible information promotes health literacy and empowers patients to actively engage in discussions about their care.
2. Educational Tools:
Empowering patients through educational tools involves the strategic use of resources to enhance their knowledge and understanding of health-related matters. This encompasses both digital solutions, such as interactive apps and online modules, and traditional methods like pamphlets or workshops. Educational tools should focus not only on specific conditions but also on promoting general health awareness. By providing patients with the knowledge they need, healthcare professionals contribute to building a foundation of informed decision-making, enabling patients to navigate their healthcare journey more effectively.
3. Communication:
Encouraging open and transparent communication between healthcare providers and patients is critical for fostering a collaborative decision-making process. This involves active listening by healthcare professionals, creating a space where patients feel comfortable expressing their concerns and asking questions. Effective communication extends to ensuring that medical information is conveyed in a language and format that patients can comprehend. In a collaborative environment, patients are not just recipients of information but active participants in discussions about their care, contributing to a shared decision-making model.
4. Digital Health Tools:
Leveraging the capabilities of digital health tools, such as apps and wearables, is instrumental in enabling continuous monitoring and providing personalized healthcare insights. These tools empower patients to actively manage their health by offering real-time data on vital signs, medication adherence, and lifestyle choices. Through features like remote monitoring and health tracking, patients gain a deeper understanding of their well-being and inprove their self-health management. Additionally, personalized insights derived from digital health tools empower patients to make informed decisions, reinforcing the connection between self-awareness and proactive healthcare management.
5. Support Networks:
Creating a supportive environment that includes family, friends, and online communities is crucial for enhancing patients’ emotional and informational support. Support networks contribute to a holistic approach to patient care, acknowledging the influence of social and emotional factors on health outcomes. Healthcare providers can facilitate the establishment of support networks by encouraging patient engagement in community-based programs, support groups, or online forums. By acknowledging the importance of emotional well-being and offering avenues for social support, healthcare professionals contribute to a patient-centred care approach that extends beyond the clinical setting.
Last words…
In the age of digital transformation, patient empowerment stands as the cornerstone of a patient-centred healthcare system. The synergy between patients and digital health tools propels us into an era where individuals actively manage their health with real-time data. The multifaceted approach—access to information, education, communication, digital tools, and support networks—provides a roadmap for fostering active patient participation. As we move toward the patient empowerment, we usher in a collaborative future in healthcare, where individuals are not just recipients but active partners in their journey to optimal health. Central to patient empowerment is the recognition that each patient is a unique individual with their own set of preferences, values, and priorities. The incorporation of patient preferences in decision-making processes is more than a courtesy; it’s a fundamental aspect of providing patient-centered care. When patients actively contribute to decisions about their healthcare, it not only aligns with their personal values but also creates a more collaborative and trusting relationship with healthcare providers. This collaborative decision-making process is intricately linked to improved health outcomes and the delivery of quality care.
References:
- Patient empowerment and health care. Available from: https://www.ncbi.nlm.nih.gov/books/NBK144022/
- Angelmar R, Bermann BP. Patient empowerment and efficient health outcomes. Financing sustainable healthcare in Europe. 2007:139–162. [accessed 26 February 2009]; http://www.sustainhealthcare.org/The_Cox_Report.pdf.
Melika Azim Zadegan works as a doctoral researcher in the Neuro-Innovation PhD programme. Her research focuses on remote iNPH patient monitoring.