Faezeh Heidari: From Seizure to epilepsy: Understanding how brain behaves in epilepsy
But what exactly are seizures and epilepsy?
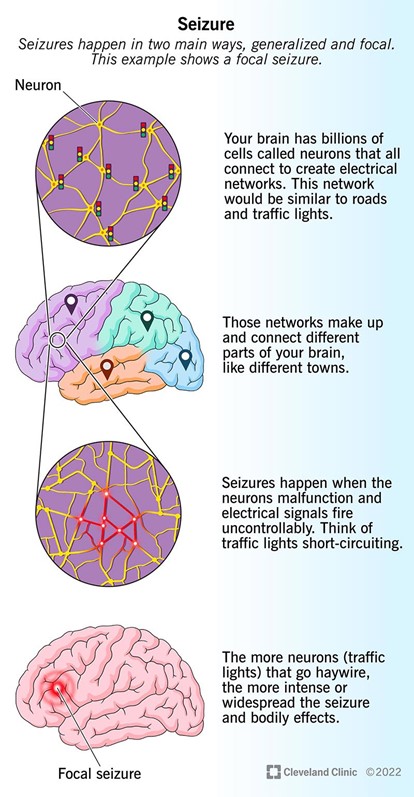
Seizures
Seizures are sudden, temporary bursts of abnormal electrical activity in the brain that disrupt the normal communication between brain cells. These disruptions can lead to sudden changes in movement, sensation, behaviour, function, or awareness.
While every brain has the potential to experience a seizure, people with epilepsy have a lower seizure threshold, making them more prone to recurrent seizures.
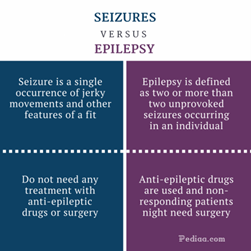
However, it’s important to note that not everyone who has a seizure has epilepsy.
Epilepsy
Epilepsy is a neurological disorder and a spectrum condition that encompasses various types of seizures and epilepsy syndromes. Individuals with epilepsy are at an increased risk of experiencing recurrent seizures.
The impact of epilepsy varies greatly from person to person and depends on factors such as:
- Type, frequency, severity, and duration of seizures
- The brain region where seizures originate
- Underlying cause of the epilepsy
- Response to anti-seizure medications, surgery, or neurostimulation treatments
- Presence of brain abnormalities
A person can experience a seizure due to an identifiable physical cause such as acute illness, trauma, fever, infection, stroke, or vascular malformation. These are known as provoked seizures and are not classified as epilepsy.
Seizure and Epilepsy difination based on ILAE (International League Against Epilepsy)
In contrast, an epileptic seizure is defined as a transient episode of signs and/or symptoms resulting from abnormal, excessive, or synchronous neuronal activity in the brain (ILAE, 2005).
Epilepsy is a chronic brain disorder characterized by a lasting predisposition to generate epileptic seizures.
Currently, epilepsy ranks as the fifth leading neurological cause of disability. It has a treatment gap of 50–75% in low- and middle-income countries, and in 2019, the global annual cost of care was estimated at approximately $120 billion.
Demographics
- Epilepsy affects approximately 70 million people worldwide, with 2.4 million new cases diagnosed each year.
- Up to 70% of individuals with epilepsy could live seizure-free if properly diagnosed and treated.
Risks and Challenges
- Increased risk of comorbidities and premature mortality (up to three times higher than the general population).
- Stigma and discrimination, affecting quality of life.
- Social and economic burdens, especially in low-resource settings.
- According to the International League Against Epilepsy (ILAE) classification, epilepsy includes a wide range of seizure types and syndromes, each associated with different comorbidities and underlying etiologies.
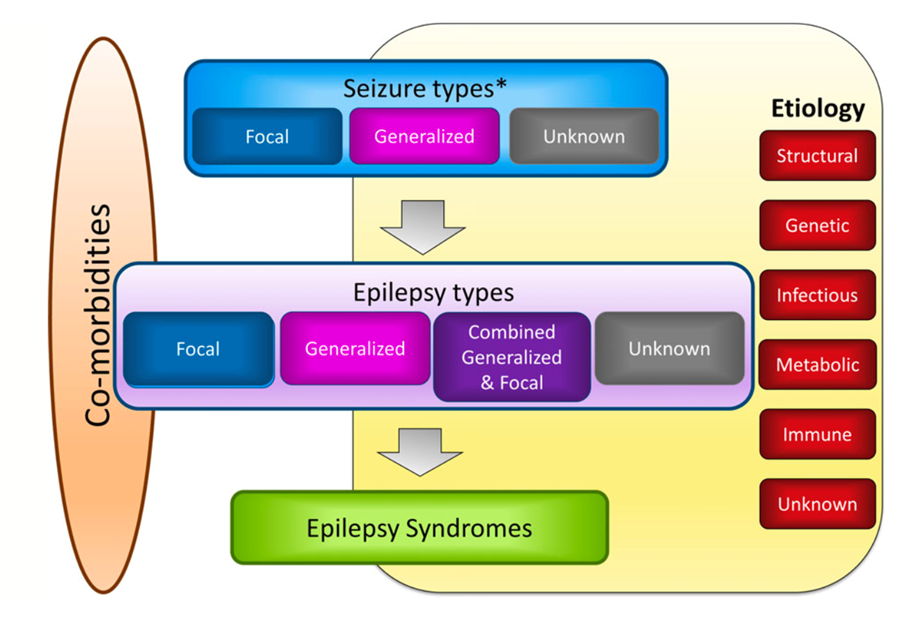
We also classify epilepsy based on how and where seizures begin:
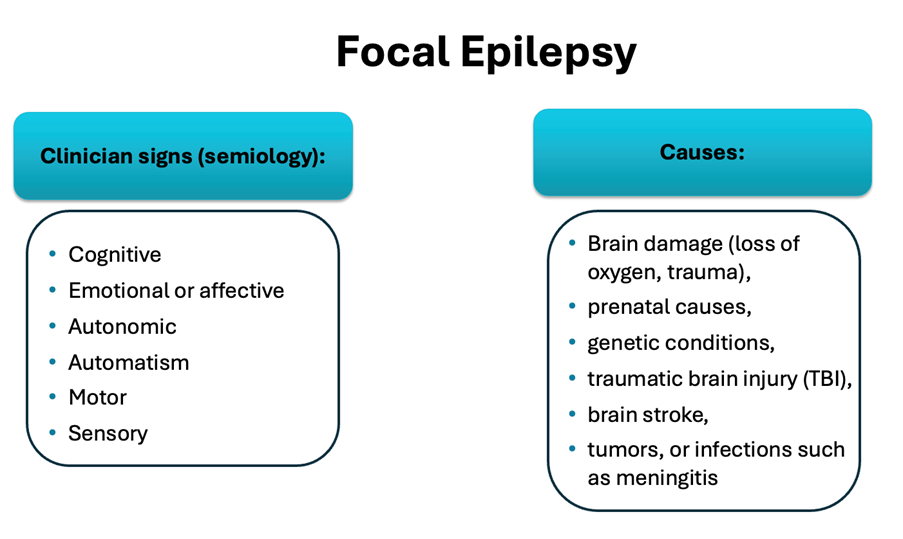
- Focal onset epilepsy starts in a specific area of the brain. Symptoms can range from mild to severe depending on how the abnormal electrical activity spreads.
- Generalized epilepsy involves both sides of the brain from the start, but some generalized seizures may begin as focal and then spread bilaterally.
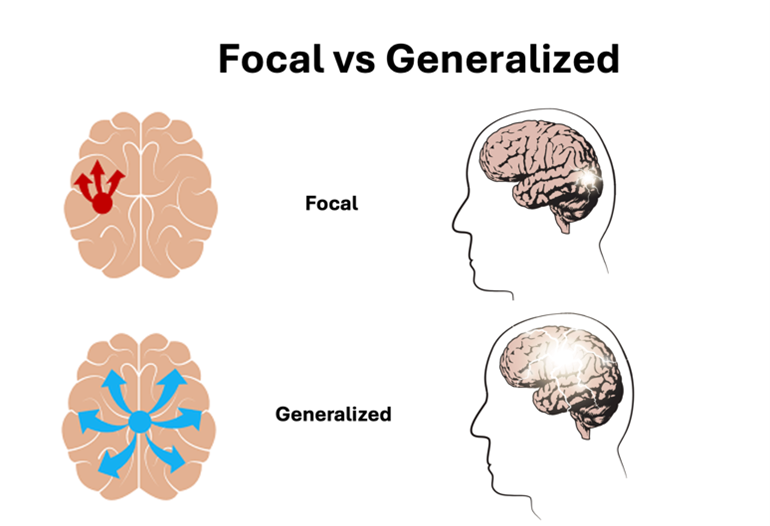
The focus of my research project is focal epilepsy and its underlying brain mechanisms, which involves seizures arising from localized regions within the brain.
Despite the availability of over 20 types of anti-epileptic drugs (AEDs), approximately 30% of patients do not achieve seizure control. These cases are classified as Drug-Resistant Epilepsy (DRE). Also referred to as refractory, intractable, or uncontrolled epilepsy defined as the failure of at least two adequate trials of anti-seizure medications to achieve sustained seizure freedom.
Treatment Options and Outcomes
- Surgical resection of the epileptogenic zone (EZ) is a key option, but only 50–70% of operated patients achieve long-term seizure freedom.
- Reliable localization of the EZ increases the chance of becoming seizure-free by up to 2.5 times.
Presurgical Evaluation Methods
- Seizure semiology (clinical observation of seizure behavior)
- Electroencephalography (EEG), including intracranial EEG (iEEG) and video-EEG monitoring
- Neuropsychological assessments
- Multimodal imaging techniques (e.g., MRI, PET, SPECT)
For drug-resistant and non-localizable cases, or when surgery fails, neuromodulation therapies such as deep brain stimulation (DBS) and vagus nerve stimulation (VNS) are considered.
References
- https://www.epilepsy.com/what-is-epilepsy/understanding-seizures
- Cho and Jang, 2020, https://doi.org/10.1038/s41598-019-56958-y
- https://www.mayoclinic.org
Faezeh Heidari works as a doctoral researcher in the Neuro-Innovation PhD Programme. Her research focuses on enhancing the identification of the epileptogenic zone.