Melika Azim Zadegan: My First PhD Study Results: Key Insights on Remote Monitoring Acceptance Among iNPH Patients in the Pre-Implantation Phase
The world is rapidly advancing toward digitalization across all sectors, and healthcare is no exception. As part of this transformation, home-based remote monitoring (RM) has emerged as a promising framework for tracking patients’ health from the comfort of their homes using digital technology. RM enables the real-time transmission of patient health data to clinical sites, offering a valuable tool for early disease detection, personalized interventions, and proactive healthcare management. It has gained traction across various healthcare contexts, including neurological conditions, as it allows for continuous monitoring without the need for frequent hospital visits.
RM is particularly appealing to elderly patients, many of whom wish to age in place and maintain their independence. By reducing hospital visits and enabling continuous health tracking, RM not only enhances clinical care but also empowers patients to take a more active role in managing their health. However, despite its growing adoption, not everyone is equally ready to embrace RM.
Who Is More Likely to Adopt Remote Monitoring?
In the first article of my PhD, we investigated whether sociodemographic factors—including age, gender, education level, living arrangements, caregiver presence at outpatient clinic visits, and place of residence—are associated with RM acceptance among elderly neurological patients, specifically those with idiopathic normal pressure hydrocephalus (iNPH) in the pre-implementation phase. iNPH is a condition characterized by a triad of symptoms: gait disturbances, cognitive decline, and urinary incontinence, often leading to a decreased quality of life and an increased need for medical support.
Why RM Matters for Elderly Neurological Patients with iNPH?
Most elderly people prefer to age in place—staying in their own homes for as long as possible. This is especially true for those with neurological conditions like idiopathic normal pressure hydrocephalus (iNPH). For these patients, RM could be a promising solution, reducing unnecessary hospital visits and ensuring timely medical attention—without waiting for their next hospital visit when symptoms might worsen.
What We Discovered: Key Factors in Remote Monitoring Acceptance in pre-implantation phase
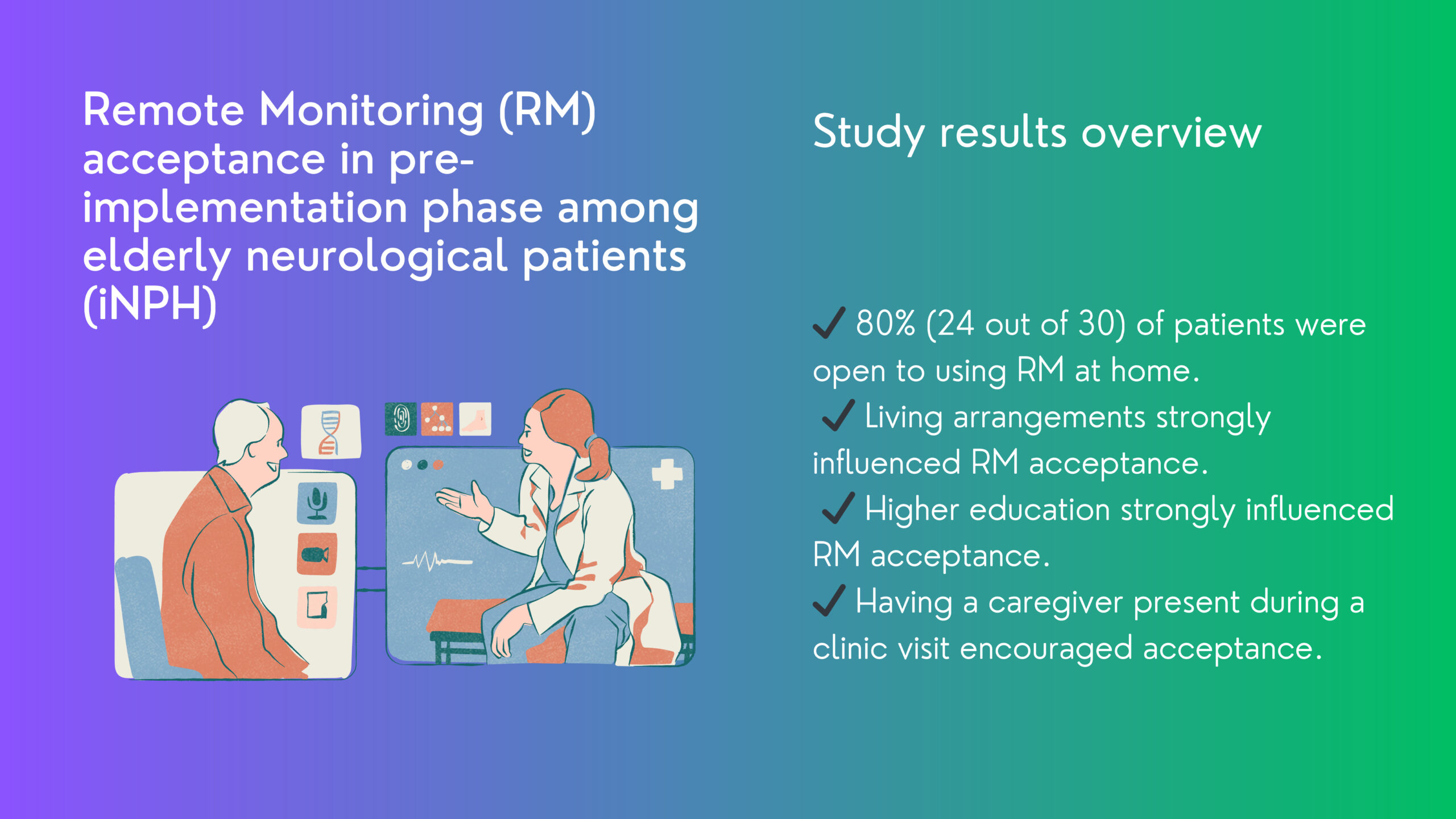
We conducted a study at Kuopio University Hospital, Neurosurgery unit in Finland, surveying 30 elderly patients about their sociodemographic factors (age, gender, education level, living with a caregiver, caregiver presence at an outpatient clinic visit, and place of residence) and their acceptance of RM (Yes/No).
Our research findings indicate that living arrangements, education level, and caregiver involvement during outpatient visits significantly influence RM adoption. Here is what we found:
Living With a Caregiver? You’re More Likely to Say Yes to RM
Elderly patients who lived with a family caregiver were significantly more likely to embrace RM than those who lived alone. This makes sense—caregivers provide both emotional and practical support, helping patients feel more comfortable with new healthcare technologies. For those who live alone, learning to use RM might feel overwhelming without additional assistance.
Higher Education = Higher RM Acceptance
Patients with higher education levels were more open to RM adoption, likely because they are more familiar with technology and digital tools. This highlights a crucial point: for RM to succeed, healthcare providers must ensure that those with lower education levels receive clear, easy-to-understand information and training.
Caregivers at Clinic Visits: A Confidence Booster?
Patients who had a caregiver present during their clinic visit were more likely to accept RM, although the result wasn’t statistically significant. However, the trend suggests an important insight: involving caregivers in RM discussions early on could help patients feel more comfortable and confident about trying it.
What Didn’t Matter as Much?
Surprisingly, some factors we expected to influence RM acceptance didn’t show a strong effect:
❌ Age – Older patients weren’t necessarily more resistant to RM.
❌ Gender – No significant differences between men and women in RM acceptance were noticed.
❌ Place of Residence – Living in a rural area didn’t make patients any less likely to accept RM, despite concerns about internet access and technology availability.
However, since our sample size was small, these results are not definitive. Future studies with larger, more diverse samples are needed to confirm these findings.
How can we improve RM Adoption? Practical Tips
Our research findings highlight the importance of considering individual circumstances when implementing digital health solutions, as certain groups may require additional support or tailored interventions to facilitate acceptance and engagement with RM technology.
Do you want to make RM work for more elderly neurological patients? Here’s our tips:
✅ Make RM Easy to Understand – Healthcare providers should offer clear, simple training on RM, particularly for patients with lower education levels.
✅ Get Caregivers Involved from Day One – Encourage caregivers to join clinic visits when RM is being discussed. Their support could make all the difference.
✅ Tailor RM Strategies – Consider individual patient needs and potential barriers to technology use, offering personalized guidance where necessary.
✅ Address Technology Concerns – Offer technical support and reassurance for elderly patients who may feel hesitant about using RM devices.
Last words?
The future of RM is bright, but it’s not a one-size-fits-all solution. Our research highlights the importance of tailoring RM adoption strategies to individual patients. If we take factors like living arrangements, education, and caregiver involvement into account before implementation, we can make RM more effective, accessible, and widely accepted.
At the end of the day, healthcare technology should adapt to patients—not the other way around! By refining RM approaches based on patient-specific needs, we can improve health outcomes and enhance the overall quality of life for elderly neurological patients.
Last but not least, I would like to express my heartfelt gratitude to my supervisors and co-authors in this study: Professor Päivi Eriksson, Dr. Eeva Aroma, Associate Professor Tero Montonen, Rosa Sählström, and Professor Ville Leinonen. Without your guidance and support, this work would not have been possible. I also extend my thanks to the NeuroInnovation PhD programme, MSCA Horizon for its invaluable support and funding for my PhD research.
Melika Azim Zadegan works as a doctoral researcher in the Neuro-Innovation PhD programme. Her research focuses on remote iNPH patient monitoring.